Sugar and Cancer

Does sugar feed cancer cells, and if so, should I completely avoid it?
Claim: Tumors prefer sugar for energy and will use more than normal cells. Consuming sugar can result in cancer growing and spreading more quickly. Avoiding all sources of sugar will inhibit cancer cells.
What is Our Recommendation?
While researchers continue to investigate the connection between sugar and cancer, there is accumulating evidence that sugar consumption is associated with increased cancer risk, recurrence, and mortality. Specifically, high blood sugar levels lead to conditions such as high insulin levels and obesity, which both increase the risk for cancer.
So, without provoking unnecessary anxiety, what can you do to keep your blood sugar balanced, maintain a healthy weight, and decrease insulin resistance?
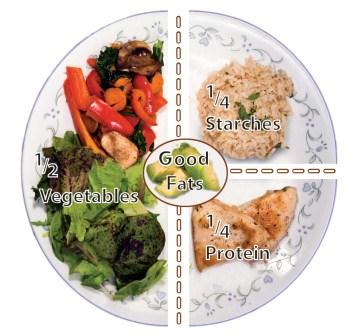
Balance Carbohydrate Intake and Keep Portion Sizes in Check
Balance each meal by keeping carbohydrate intake to ¼ of the plate, protein to ¼ of the plate and fill the remaining ½ of the plate with colorful, low glycemic veggies. If possible, avoid eating a carbohydrate by itself. Even at snacks combine your carbohydrate with a small amount of protein or healthy fat.
Choose High Quality Complex Carbs
Choose high fiber starches as close to their natural form as possible when choosing carbohydrates. This includes such foods as stone ground whole wheat, barley, steel cut oats, legumes, crunchy and leafy veggies, and most fruit (but not fruit juice). Using tools like the Glycemic Index (GI) and Glycemic Load (GL) can be helpful in choosing carbohydrates. Read labels carefully. The higher an ingredient appears in the ingredient list, the greater the amount is present in the food. Also beware of all the different forms of hidden sugar; corn syrup, barley malt, dextrose, fruit juice concentrate, maltose, maltodextrin, dextrin, brown rice syrup, sorbitol, evaporated cane juice, mannitol, honey, maple syrup, molasses, beet sugar, agave nectar, etc.
- Best Choice: Low GI Foods = 0 – 54 / Low GL Foods = 0-10
- Moderate: Medium GI Foods = 55 – 69 / Medium GL Foods = 11-19
- Limit: High GI Foods = GI of 70+ / High GL Foods = 20+
| Low GI / GL | Medium GI / GL | High GI / GL |
| Stone ground whole wheat, pumpernickel bread, dark rye | Sourdough, oat bran, multi-grain, pita breads | French bread, white bread, bagels, English muffins |
| Popcorn, whole grain crackers | Rice cakes, pretzels, Saltine crackers, corn chips, graham crackers, vanilla wafers | |
| Rolled / steel cut oats | Quick oats | Instant oatmeal |
| All bran cereal | Shredded Wheat, Special K, Muesli | Flaked or puffed cereals, rice or oat cereal, Grape Nuts |
| Barley, bulgur, brown rice, whole wheat pasta, white pasta al dente | White rice, couscous, white Basmati rice, quinoa | Short-grain sticky rice |
| Most vegetables, including yams, carrots and peas | Sweet potatoes, corn, winter squash, new boiled potatoes | Russet or instant potatoes |
| Most fruit, including bananas | Tropical fruits, dried fruit | |
| Beans and lentils, hummus | Baked beans | |
| Soy milk, milk, yogurt | Custard, ice cream |
Extensive Charts
- Glycemic Index & Glycemic Load for 100 Foods (Harvard Medical School)
- Glycemic Index & Glycemic Load Table (American Journal of Clinical Nutrition)
Limit Simple, Refined Sources of Sugar
Avoid sugary drinks and choose whole fruit over fruit juice. Limit sweets, such as ice cream, candy, pastries, cookies, etc. to occasional treats; not everyday foods. Have a piece of fruit or a square of dark chocolate (>70%) for dessert.
Based on information gathered from the CDC’s National Health and Nutrition Examination Survey 2003-2010, the following table shows the percentage of total added sugar found in the American diet (22):
| Age 20-50 | Age >50 | |
| Soda / Sugar-Sweetened Beverages | 40.2% | 21.0% |
| Desserts: Grain Based | 11.4% | 17.5% |
| Fruit Drinks | 7.7% | 5.4% |
| Candy | 5.9% | 7.4% |
| Dessert (Dairy-Based) | 4.4% | 8.3% |
| Tea | 4.7% | 4.9% |
| Cereals | 3.0% | 3.7% |
| Sugar & Honey | 4.3% | 5.5% |
Spice It Up
Include herbs and spices in your cooking that may have an effect in lowering blood sugar: cinnamon, fenugreek, onions, garlic, chives, leeks, bay leaf, and cloves.
Move More
Exercise decreases insulin resistance and can help your body use up circulating glucose; in addition to helping you maintain a healthy weight. Move in some way every day. Aim for 30 minutes or more of moderate activity most days of the week.
For additional information regarding sugar and health, visit the Sugar Science website.
What is the Evidence?
Biology:
- Many cancer cells do selectively depend on glucose for energy and some estimates suggest they use 50-100x more glucose than normal cells (1). For this reason, many researchers are looking at ways to target glycolytic metabolism with medications, like metformin (2).
- It’s important to note that although cancer cells utilize glucose for energy, all macronutrients can be used as fuel for both healthy and cancerous cells. Total caloric intake can also play a role in cancer cell proliferation. We will look at this topic further in the FAQ on calorie restriction and fasting.
- High fructose intake may also contribute to increased risk of cancer. Unlike glucose, fructose bypasses the normal phosphorylation process in the liver becoming a substrate for aldolase and producing very high levels of ATP and citrate. ATP and citrate go on to make fatty acids; which means that overall more fat is made from fructose than glucose. Increased fat storage leads to obesity, which leads to insulin resistance and the increased risks described above. This pattern seems to be especially true with high fructose corn syrup (1). Fructose is also the principal sugar in fruit. However, fruit has high fiber content and therefore a lower glycemic load than sugary foods and drinks sweetened with high fructose corn syrup. As an example, you would probably have to eat about a bushel (or 48 pounds) of apples to get the same amount of fructose found in a 40 oz Coke.
Clinical:
- A retrospective study of newly diagnosed patients with Grade 4 Glioblastoma showed a direct correlation between survival time and blood glucose levels (3). The study was conducted between the years 1999-2004 with 191 patients. Patients were untreated except for biopsy and glucocorticoid administrations. Patients received radiation during the study. Results were adjusted for mean daily glucocorticoid dose, age, and baseline performance score. The researchers found that higher blood glucose levels were associated with shorter survival times.
- An epidemiological cohort study with over 60,000 Swedish women (part of the Swedish Mammography Cohort) found that women consuming high glycemic load diets were more likely to develop breast cancer; particularly estrogen-receptor positive cancer (4). In this same cohort of women, the investigators also found that those with the highest intake of sugar, more than 35 grams per week plus consumption of pastries and cookies more than 3 times per week, had a statistically significant increased risk of endometrial cancer (5).
- Similar findings were demonstrated in an observational study of more than 1000 stage-3 colon cancer patients. Those with diets with the highest glycemic load and total carbohydrate intake had a statistically significant increased risk of both recurrence and mortality, with worse disease-free survival among overweight or obese patients (6). In this same cohort of patients, the investigators found that those with an intake of 2 or more 12 oz. servings of sugar-sweetened beverages per day had a significantly increased risk of both recurrence and mortality (7).
- A case-controlled population study, conducted in Malaysia, with 382 breast cancer patients and 382 controls showed a 2-fold increased risk of breast cancer among both pre and post-menopausal women who had the highest intake of sugar (more than 61 grams, or 15 tsp, per day) (8). There was no association observed between total carbohydrate intake and cancer risk. The investigators concluded that this was most likely due to the fact that the Asian Diet is typically high in carbohydrates.
- The fact that cancer cells depend on readily available glucose may explain why epidemiological evidence has shown that diabetics are more prone to cancer; particularly of the breast, colon, prostate, liver, and pancreas.
- Most of the components of metabolic syndrome (Figure 1) have individually been linked to cancer in some way; BMI >25, increased waist circumference, high blood glucose levels, high triglyceride, and low HDL levels. Two studies in particular have shown that clustering of these components significantly increases the risk of colon cancer mortality compared with the individual components. The underlying mechanisms for this increased risk are thought to be related to insulin resistance, aromatase activity, adipokine production, angiogenesis, glucose uptake, and oxidative stress/DNA damage to cells (11).
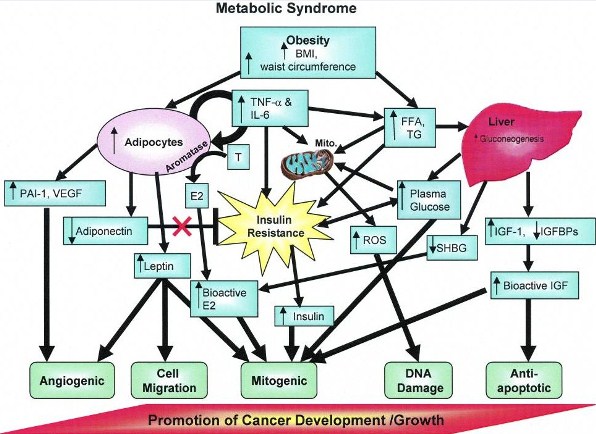
Figure 1: Diagram of factors linking Metabolic Syndrome with cancer development. Plasma glucose, BMI/waist circumference, and triglycerides/FFA affect different complementary processes that can work together to promote cancer development/growth. Additional characteristics of the MS, such as increased HDL and hypertension, are also correlated with cancer growth, but a direct mechanism for these associations has not been confirmed. Abbreviations: E, estrone; E2, estradiol; A, androgens; mito, mitochondria; ROS, reactive oxygen species; SHBG, sex hormone-binding globulin; FFA, free or nonesterified fatty acids; TG, triglycerides; IGFBPs, insulin-like growth factor-binding proteins (11).
- According to results from several cohort studies looking at Glycemic Index (GI), Glycemic Load (GL) and Cancer Risk, higher dietary GI and dietary GL are associated with an increased risk of certain digestive and hormonally related cancers: colorectal, endometrial, breast, and pancreatic in particular (12, 13, 14, 15).
- Hyperglycemia (high blood sugar levels) may increase DNA mutations, increase tumor survival, increase proliferation and increase invasion and migration of cancer cells (Figure 2) (16). The indirect effects of this may be from increased insulin and IGF. Insulin is an especially powerful growth stimulant for breast, prostate, and colon cancer cells (17, 18). This may be because some types of cancer cells (e.g., breast cancer cells) have more insulin receptors on their surface allowing them to respond more than normal cells to insulin’s ability to promote growth (19). IGF-1 has been shown to encourage the growth of tumors of the prostate, colon, lung, pancreas, and breast through promoting angiogenesis and metastasis (20, 21).
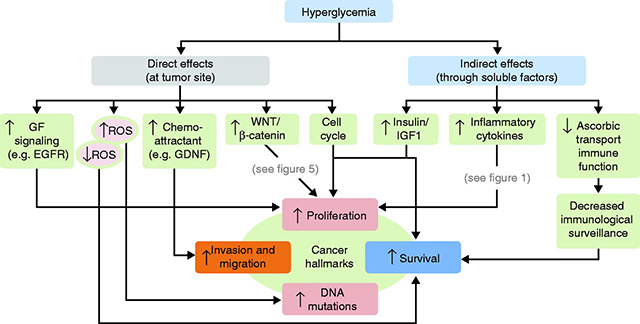
Figure 2: The many mechanisms by which hyperglycemia may feed cancer cells. Hyperglycemia may have direct effects on the tumor site or indirect effects through soluble factors. To view the additional figures listed in the diagram refer to the Garcia-Jimenez study. Both direct and indirect effects converge on cancer hallmarks (increased proliferation, survival, invasion, and migration and accumulation of mutations in the DNA) (16).
References:
1. Cantley LC. Cancer, metabolism, fructose, artificial sweeteners, and going cold turkey on sugar. BMC biology 2014;12:8.
2. El Mjiyad N, Caro-Maldonado A, Ramirez-Peinado S, Munoz-Pinedo C. Sugar-free approaches to cancer cell killing. Oncogene 2011;30:253-64.
3. Derr RL, Ye X, Islas MU, Desideri S, Saudek CD, Grossman SA. Association between hyperglycemia and survival in patients with newly diagnosed glioblastoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2009;27:1082-6.
4. Larsson SC, Bergkvist L, Wolk A. Consumption of sugar and sugar-sweetened foods and the risk of pancreatic cancer in a prospective study. The American Journal of Clinical Nutrition 2006; 84: 1171-6.
5. Friberg E, Wallin A, Wolk A. Sucrose, high-sugar foods, and risk of endometrial cancer–a population-based cohort study. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 2011;20:1831-7.
6. Meyerhardt JA, Sato K, Niedzwiecki D, et al. Dietary glycemic load and cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. Journal of the National Cancer Institute 2012;104:1702-11.
7. Fuchs MA, Sato K, Niedzwiecki D, et al. Sugar-sweetened beverage intake and cancer recurrence and survival in CALGB 89803 (Alliance). PloS one 2014;9:e99816.
8. Sulaiman S, Shahril MR, Wafa SW, Shaharudin SH, Hussin SNAS. Dietary Carbohydrate, Fiber and Sugar and Risk of Breast Cancer According to Menopausal Status in Malaysia. Asian Pacific Journal of Cancer Prevention 2014;15:5959-64.
9. Tsugane S, Inoue M. Insulin resistance and cancer: epidemiological evidence. Cancer science 2010;101:1073-9.
10. Myers AP, Cantley LC. Sugar free, cancer free? Nutrition 2012;28:1036.
11. Cowey S, Hardy RW. The metabolic syndrome: A high-risk state for cancer? The American journal of pathology 2006;169:1505-22.
12. George SM, Mayne ST, Leitzmann MF, et al. Dietary glycemic index, glycemic load, and risk of cancer: a prospective cohort study. American journal of epidemiology 2009;169:462-72.
13. Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, Brand-Miller JC. Glycemic index, glycemic load, and chronic disease risk: a meta-analysis of observational studies. The American Journal of Clinical Nutrition 2008; 87: 627-37.
14. Gnagnarella P, Gandini S, La Vecchia C, Maisonneuve P. Glycemic index, glycemic load, and cancer risk: a meta-analysis. The American Journal of Clinical Nutrition 2008; 87: 1793-801
15. Hu J, La Vecchia C, Augustin LS, et al. Glycemic index, glycemic load and cancer risk. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO 2013;24:245-51.
16. Garcia-Jimenez C, Garcia-Martinez JM, Chocarro-Calvo A, De la Vieja A. A new link between diabetes and cancer: enhanced WNT/beta-catenin signaling by high glucose. Journal of molecular endocrinology 2014;52:R51-66.
17. Goodwin PJ, Ennis M, Pritchard KI, Trudeau ME, Koo J, Madarnas Y, Hartwick W, Hoffman B, Hood N. Fasting insulin and outcome in early-stage breast cancer: results of a prospective cohort study. Journal of Clinical Oncology 2001; 20: 42-51.
18. Hammarsten J, Hogstedt B. Hyperinsulinaemia: a prospective risk factor for lethal clinical prostate cancer. European journal of cancer 2005;41:2887-95.
19. Papa V, Pezzino V, Costantino A, Belfore A, Giuffrida D, Frittitta L, Vannelli GB, Brand R, Goldfine ID, Vigneri R. Elevated insulin receptor content in human breast cancer. Journal of Clinical Investigation 1990; 86: 1503-1510.
20. Fürstenberger G, Senn H-J. Insulin-like growth factors and cancer. The Lancet Oncology 2002;3:298-302.
21. Boyd DB. Insulin and cancer. Integrative cancer therapies 2003;2:315-29.
22. Drewnowski A, Rehm CD. Consumption of added sugars among US children and adults by food purchase location and food source. The American journal of clinical nutrition 2014;100:901-7.
Legal notice
This documentation has been compiled by the UCSF Osher Center with all due care and expert knowledge. However, the UCSF Osher Center provides no assurance, guarantee or promise with regard to the correctness, accuracy, up-to-date status or completeness of the information it contains. Readers are strongly advised to discuss the information with their physician. Accordingly, the UCSF Osher Center shall not be liable for damage or loss caused because anyone relies on the information.